The treatment of antibodies could block toxin derived from the intestine behind renal fibrosis

An intestinal microbe molecule causes diabetic kidney scars. The blocking can offer new treatment options.
A new study by the University of Illinois Urbana-Champaign and the MIE university in Japan has revealed that a molecule produced by intestinal bacteria can go to the kidneys, where it triggers inflammation, tissue scars and fibrosis. These processes represent a serious complication of diabetes and are among the main causes of renal failure.
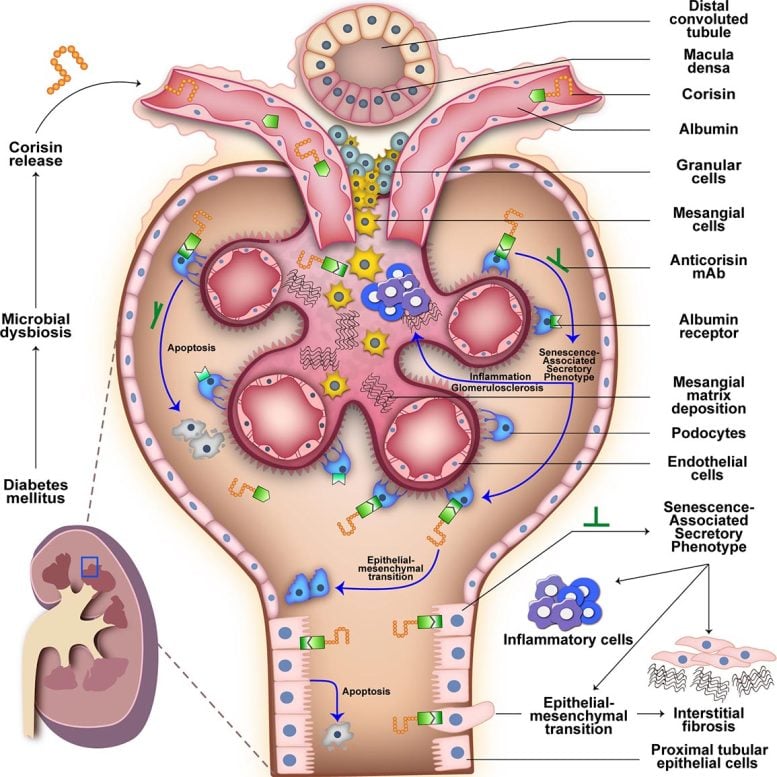
The molecule, known as Corisin, is a small peptide generated by Staphylococcus bacteria in the intestine. Researchers have detected high levels of Corisine in the blood of patients with diabetic renal fibrosis. To understand its role, they combined computer simulations with experiences of fabric and mice, tracing the way Corisin moves from the intestine to the kidneys, how it causes kidney damage and how antibody -based treatments could help block its harmful effects.
“Our previous studies have shown that Corisin can damage cells and worsen scars and tissue fibrosis in other organs, we therefore suspected that it could be a hidden driver of kidney fibrosis,” said the Illinian Illinology Professor Animal Sciences, Isaac Cann, who led the study with the Immunology Professor MIE, Esteban Gabazza. Cann and Gabazza are affiliates of the Carl R. Woese Institute for the genomic biology of Illinois. “Our new discoveries suggest that Corisin is indeed a hidden blow behind progressive renal damage in diabetes, and that blocking could offer a new way of protecting kidney health in patients.”
The researchers published their results in the journal Nature communications.
A hidden driver of diabetic kidney damage
Dr. Taro Yasuma of Mie University, doctor and first author of the study, explained that diabetic kidney fibrosis is one of the main causes of renal failure in the world. Despite its impact, the main factors behind the condition have remained clear and there is currently no therapy that can stop its progression.
“Many people with long-standing diabetes finally develop renal fibrosis, and once it is progressing, there are limited options beyond dialysis or renal transplantation.

To investigate more, the team analyzed blood and urine samples of patients with a diabetic kidney disease. Their results have shown that these patients had much higher levels of Corisin compared to healthy individuals, and that the concentration of Corisin in the blood was directly linked to the severity of kidney lesions.
Corisin monitoring of the intestine to the kidneys
By seeing the same results in mice with renal fibrosis, the researchers followed what Corisin did in the kidneys of the mice. They found that Corisin accelerates aging in kidney cells, triggering a chain reaction from inflammation to cell death to an accumulation of scar tissue, ultimately resulting in the loss of kidney function and aggravation of fibrosis.
But how did Corisin go from the intestine to the kidneys? The groups of Cann and Gabazza collaborated with U. of I. They found that Corisin can settle in albumin, one of the most common proteins of blood, and cross it in the bloodstream. When he reaches the kidneys, Corisin stands out from albumin to attack delicate structures that filter blood and urine.

The treatment of antibodies is promising
To confirm that Corisin was the main culprit behind kidney damage, the researchers gave mice antibodies against Corisin. They saw a spectacular reduction in the speed of kidney damage.
“When we have treated mice with an antibody that neutralizes Corisin, it has slowed the aging of kidney cells and considerably reduced kidney healing,” Gabazza, who is also an auxiliary professor of Animal Sciences at Illinois, said. “Although no antibodies of this type are currently approved for use in humans, our results suggest that it could be developed in a new treatment.”
Then, the researchers plan to test anticorisin treatments in more advanced animal models, such as pigs, to explore how they could be adapted for safe use in humans. READ. of I. and MIE University have joint disclosure of invention on Corisin antibodies.
“Our work suggests that the blocking of Corisin, with antibodies or other targeted therapies, could slow down or prevent kidney scars in diabetes and thus improve the quality of life of patients,” said Cann.
REGRETION: “Cooperation and decrease fractions are separated, this is the only way. Nature communications.
Two: 10.1038 / S41467-025-61847-2
This study was supported by the Japan Science and Technology Agency, the Japan Society for the Promotion of Science, La Takeda Science Foundation, the Japan Association for Diabetes Education and Care, the Grant Eli Lilly Japan Innovation Research, the Daiwa Security Foundation and the Charles and Margaret Levin Family Family.
Never miss a breakthrough: join the Scitechdaily newsletter.

:max_bytes(150000):strip_icc()/VWH-GettyImages-1070970608-c897a6b08f3b40b79d403d4615d76ebd.jpg?w=390&resize=390,220&ssl=1)


:max_bytes(150000):strip_icc()/Health-GettyImages-2165148699-c2eb08c18e974bb49f795f84dbbb031d.jpg?w=390&resize=390,220&ssl=1)