GOP talking point argues ACA is haunted by ‘ghost’ enrollees, but the devil is in the data

The idea that the Affordable Care Act marketplaces are riddled with fraud has become a major talking point among Republicans, as lawmakers in Congress weigh whether to extend enhanced tax credits that help offset the cost of health care marketplace coverage for low- and middle-income people. These ACA grants expire at the end of the year and have become a flashpoint in the government funding showdown.
“Tax credits rightly benefit some people. And we think tax credits actually create a lot of waste and fraud within the insurance industry,” Vice Chairman JD Vance said in a recent interview on CBS News. “We want to make sure the tax credits benefit the people who need them. »
Key to the Republican argument that fraud is widespread is a report released in August by the Paragon Health Institute, a Republican-aligned think tank. The report focuses on “ghost enrollees” in the ACA marketplaces.
Paragon President Brian Blase said these “ghost enrollees,” who use no medical care in a year, exceed the percentages of “what would be expected in a normal, functioning health insurance market.”
Blase and his team say they quantified the percentage of claim-free enrollees in the ACA marketplace by analyzing data from the Centers for Medicare & Medicaid Services released in August.
This highlights one of the central problems with CMS data: It tracks the number of plan enrollments rather than individual enrollees.
Federal data analyzed by Paragon could count enrollees twice if they changed plans during the year, said Cynthia Cox, vice president and program director on the ACA at KFF, a nonprofit health news organization that includes KFF Health News.
According to this data, in 2021, the percentage of registrations without any medical claims was 19%. This percentage increased to 35% in 2024.
For Blase and Paragon, this increase in registrations without complaints is proof of fraud. This indicates, they say, that dishonest insurance brokers are recruiting people who don’t exist, aren’t eligible, or have other insurance and don’t need ACA coverage.
“Basically what happened was the insurers benefited, the brokers benefited financially, and a tremendous number of people were enrolled in the program,” Blase said. That’s where these ghosts come in. “They have no idea that they are registered and, as such, they do not use any medical care. »
In 2021, former President Joe Biden signed into law the American Rescue Plan Act, which provided enhanced ACA subsidies that made the plans available at low or no cost to some low-income people and expanded eligibility for subsidies to some middle-income people. These credits were extended through 2025 as part of the Inflation Reduction Act, signed into law in 2022.
The news reports show how easy it could be for insurance brokers in some states to enroll people in ACA insurance plans at no cost, without consumers’ knowledge. The Department of Health and Human Services has attempted to crack down on these fraudulent practices.
But health policy experts and analysts have cautioned against reading too closely into the number of claim-free enrollees.
“It’s not that he’s wrong, but I think he’s overinterpreting,” Michael Cannon, director of health policy studies at the libertarian Cato Institute, said of Blase’s analysis.
Cox said there is evidence that plan switching has increased, in part due to extended open enrollment periods. Increased plan switching could result in higher double-counting in federal data and increase the percentage of claim-free enrollees over the years. Some enrollees may also have participated in an ACA plan for only part of the year, which would make them less likely to file a claim.
“We’re not trying to pretend there’s no fraud. It’s a real thing. But the question is, how big is this problem?” Cox said. “Simply suggesting that anyone who doesn’t use health care is a fraudulent enrollee – that’s not true. A lot of people don’t use health care.”
It’s not uncommon for healthy people in the insurance market to not use their insurance in a given year, according to health policy experts. And thanks to the ACA’s enhanced subsidies, more people have signed up for marketplace coverage. Enrollment data shows that this has rejuvenated the market population and that younger enrollees may be less likely to use their insurance. A recent report found that each year from 2018 to 2022, an average of 23% of enrollees in employer-sponsored plans did not use their health insurance.
“In some ways the idea that people not using health insurance is some kind of problem, maybe it is. But in principle it’s not,” said Joseph Antos, a health policy expert and senior fellow at the right-leaning American Enterprise Institute. “The fact is, for insurance to work, you need people who are not making insurance claims.”
The major trade associations for insurers and hospitals, AHIP and the American Hospital Association, also took issue with Paragon’s characterization of the federal data and even published blog posts breaking down their arguments. AHIP pushed back against the idea that the insurance industry benefits from increased subsidies by saying existing law caps health plan profits.
Paragon was launched by Blase in 2021 and has become very influential in Republican health policy circles. The organization’s alumni are on staff in the Trump administration and House Speaker Mike Johnson’s office, so it follows that the group’s teachings would become Republican talking points.
It’s also nothing new for the Republican Party to say that government programs are filled with fraud. During negotiations over the One Big Beautiful Bill, Republican lawmakers insisted that Medicaid would not be cut to fund the tax cuts, but that “waste, fraud and abuse” in the health program would be eliminated.
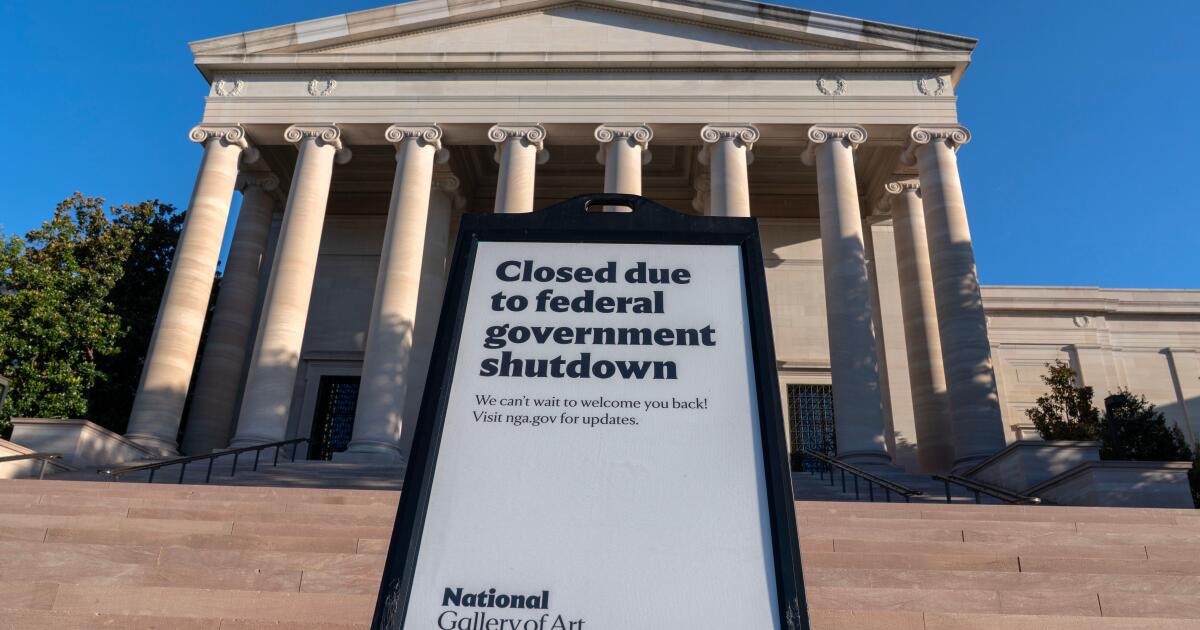
Today, the ACA is at the center of the current federal government shutdown, with Democrats pushing for Congress to extend the current ACA subsidies, which are set to expire at the end of the year. And fraud, once again, is the centerpiece of the Republicans’ argument. Democrats have a different view on the extent of fraud in the program, instead emphasizing that expiring subsidies will increase insurance premiums.
“It’s become a mess. It’s a subsidy for the insurance companies,” President Johnson said of the ACA subsidies at a press conference on the shutdown last week. “When you subsidize the health care system and pay more to insurance companies, prices go up. That’s the problem.”
KFF Health News senior correspondent Julie Appleby contributed to this report.
KFF Health News is a national newsroom that produces in-depth journalism on health issues and is one of KFF’s primary operating programs, an independent source of health policy research, polling and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).